Story highlights
Since 1988, just over 1,000 people have undergone heart-lung transplants in the US
Spencer Kolman needed the surgery due to pulmonary fibrosis caused by cancer treatment
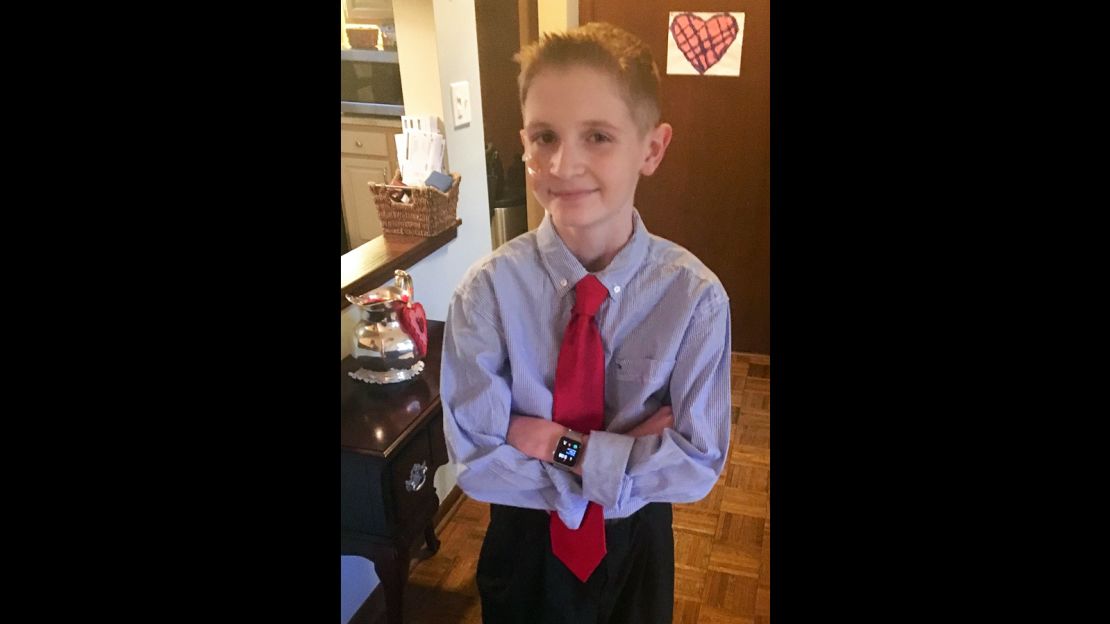
“I want to do more stuff,” Spencer Kolman said. His voice was a whisper, a painful-to-hear rasp across the telephone line.
“I’m a Boy Scout, so I want to go back and get my Eagle Scout and do … the more physical activities that I had to basically stop doing because I couldn’t keep up,” the 15-year-old said.
“I want to join the school band. I want to get back into playing the trumpet. … I did trumpet for four years, and then in eighth grade, it got tough keeping up,” he said.
“Keeping up” is Spencer’s constant refrain. Despite his best efforts, keeping up had become impossible.
“One of my friends from school and I did a radio show. Eventually, we started having to do more of just playing music because I would get out of breath,” he said.

His father’s words echo Spencer’s memories: “He needed a mobility scooter to go around school. He could only go to school for half a day because of how exhausted he was. He had to live in his room, because even getting up and going to the bathroom took so much energy out of him.”
Meanwhile, Spencer continues his litany of activities: He wants to return to his theater group. He wants to go camping. He wants to hike.
Why are his deferred dreams suddenly possible?
On November 29, Spencer received a heart-lung transplant at St. Louis Children’s Hospital’s Heart Center – the only pediatric heart-lung transplant surgery performed in the United States that year.
“He’s like a brand-new kid,” Ken Kolman said. “It’s totally amazing.”
Odyssey
Some patients make their way through a diagnostic odyssey in which they are treated for the wrong disease until their real problems are detected. Other patients make their way through a specialist odyssey: They know what’s wrong, but they cannot find a doctor who will treat them.
The Kolman family journeyed down both paths.
Their diagnostic odyssey began more than four years ago, in January 2013.
“I was playing ice hockey, and I collapsed on the ice because I was getting short of breath,” Spencer said. “Then, I basically collapsed out of exhaustion.”
The family pediatrician thought Spencer had asthma.
“So they gave me an inhaler to try, and I tried that, and it didn’t make much of a difference at all,” Spencer said. “So then we went to the University of Chicago to see what they thought.”
The verdict was walking pneumonia. This time, he was given antibiotics.
“That didn’t really do anything either,” Spencer said. At this point, more tests were done. “Eventually, they came to the conclusion that it was pulmonary fibrosis.”
Pulmonary fibrosis is when the deep tissues of the lung become thick, stiff and scarred, interfering with a person’s ability to breathe.
In most cases of pulmonary fibrosis, doctors do not understand what has caused it, but in Spencer’s case, the cause was clear. In 2002, when he was just 16 months old, Spencer was diagnosed with a form of cancer known as rhabdomyosarcoma. These cancers grow in connective tissues, such as muscles, fat, bones or the linings of joints.
Rhabdomyosarcoma is most common in children, though the disease can occur in adults.
Spencer’s cancer treatment lasted a year and called for chemo, surgery and radiation, followed by more chemo.
“Luckily, he has no memory of going through all of this,” said his father.
Considered to be in remission, Spencer remained unbothered by any cancer-related health complaints until his doctors connected the dots from chemotherapy as a baby to the scar tissue in his lungs as a teen.
By this point, three years had passed since Spencer collapsed on the skating rink. Yet it was another bleak day in January when his doctors suggested that his failing heart and two lungs required a transplant.
“We’re from Chicago, Chicago area. There are no hospitals around us that do pediatric heart-lung transplants, so I was given a list of like five hospitals in the whole United States that do this sort of surgery,” Ken Kolman said.
With relatives “out east,” the Kolman family began their search at Boston Children’s Hospital.
“They did a whole workup on him, and they said the good news was that he only needed a lung transplant, that his heart was actually better than they had thought,” Kolman said.
This unanticipated good news was followed by the heartbreak of bad news.
“They were not going to do the surgery,” Kolman said. “The lining of his lungs had almost become attached to his chest wall due to inflammation and scarring.”
Doctors at Boston Children’s worried Spencer might die on the operating table and so considered the operation “too much of a risk.”
Still, when it’s your kid, “you’d never give up hope and basically exhaust every avenue possible to help him get what he needed … to survive,” Kolman said.
And so the family tried again, this time at St. Louis Children’s hospital.
They came down from Chicago for a week in September when the hospital conducted its evaluation of Spencer.
“We were told the unfortunate news that his heart was worse than before and that he would need both a heart and lung transplant,” Kolman said. “That was a complete shock to us.”
“We thought this was it – there was no hope for our son,” he said.
Medical decision
According to Dr. Stuart Sweet, a pediatric pulmonologist and medical director of St. Louis Children’s Pediatric Lung Transplant Program, Spencer was an unusual case in that “by the time he got to us, he was a little sicker than we would like.”
“Although we consider other peoples’ opinions when we evaluate patients, we evaluate patients on our own set of criteria,” Sweet said. The hospital’s criteria “reflect our determination that a patient will benefit from the operation we’re providing them” and take into account whether there are “significant risks.”

“The concerns raised elsewhere did not really apply to our expertise or our approach, so it really was not a difficult decision for us medically,” Sweet said.
“What we don’t want to do is take a child who is so sick that we’re unlikely to get organs in time to save their life and to put them through that level of support and complexity for no good reason,” Sweet said. “The main question really was: Would we be able to get him organs in time to transplant?”
That’s always an unpredictable scenario, explained Sweet, but generally they try to give children the benefit of the doubt.
From the perspective of Dr. Pirooz Eghtesady, cardiothoracic surgeon-in-chief at St. Louis Children’s Hospital, the Kolman family “came to us expecting we would say ‘no.’ ”
“I looked at the information and disagreed with the assessment that had been made by the other institutions,” said Eghtesady, who headed the team that actually performed Spencer’s operation. “They thought the surgery was going to be prohibitively risky, extremely difficult, and that was not my assessment.
“I don’t completely fault the other institutions,” Eghtesady said, explaining that Spencer had “dense scar tissue.” Unlike other hospitals, St. Louis had become comfortable, over time, with performing this form of difficult, complicated surgery.
“About 75% of the cases that we do are redo lung transplants,” Eghtesady said, explaining that when a transplant fails a second transplant can be done in some cases.
And so St. Louis Children’s Hospital decided it would take on Spencer as a patient.
A twist of fate
“All of a sudden, he’d been given a chance,” Ken Kolman said. “So we decided to make arrangements to come down to St. Louis.”
Spencer needed to be close enough to the hospital in case a lung and heart donation became available. “According to the doctors, you only have so much time, and when they say jump you have to jump,” Kolman said.
The time between January, when the Kolman’s first learned of Spencer’s need for transplant surgery, and November when the operation happened, was “devastating” for all involved, according to Kolman. Not only was Spencer’s health getting worse, but the family, including Spencer’s 16-year-old brother, Zach, and 7-year-old sister, Evangeline, was feeling the strain.
“My wife was sacrificing time from our other son, our daughter, me, her job, too,” Kolman said. “We didn’t want to uproot everyone to move here, so we figured out a plan where my wife would move down here with Spencer and do all the prerequisite physical therapy and labs before the transplant and I would stay back home for work.”
“I was the major breadwinner, and I was the one who had all the insurance through my employer,” Kolman said. “Once I told my employer, three days later, they let me go from my job.”
“It was very hard, because the company I worked for knew of my son’s situation and had met him personally … and they just pulled the rug out from under our feet,” said Kolman, formerly a production supervisor for a small manufacturing company.
Ken and his wife, Elizabeth, 45, decided she would continue working as an assistant store manager for Walgreens, which provided insurance. And Ken moved to St. Louis with Spencer instead.
The hospital’s plan for Spencer was to treat him as an outpatient while placing him on the wait list for an organ. That way, they could bring him in for the surgery once donor organs became available.
Overall, the expectation was that Spencer’s disease would progress slowly.
“From September to the beginning of November, little by little, I could tell my son’s condition was getting worse,” Kolman said.
“We came (to St. Louis) on a Thursday, and I called Friday morning to talk to someone on the transplant team to assess him,” he said. Spencer was on 15 liters of oxygen per minute, “a crazy amount of tanks,” he said.
“Some of the doctors who had never seen him before saw him, and they were totally blown away and terrified that he was going to pass away within 24 hours,” Kolman said. They were surprised that he could survive breathing the way he had been.
“I was told if he was a normal healthy person, we’d be dead in 30 minutes or less,” he said.
Spencer entered the hospital on Friday, and by Monday, the team had put him on the wait list. By the end of the week, though, his condition had become grave, and the team was not sure he would make it.
Waiting for organs
According to Eghstedy, heart lung transplants are generally “a challenging sort of situation.” Needing a donation of both organs usually means the patient is suffering more extensive disease.
“In Spencer’s case, honestly, he was at death’s door,” Eghstedy said.
According to Sweet, Spencer was “really sitting on an edge,” but waiting for both organs, heart and lungs, can take time.
For children, “it’s generally very difficult to match a heart and lung or other multiple organ pairs,” Sweet said. Kids are “growing and developing in the period of time after they’ve received the transplant, and so it’s important for us to choose lungs that are gonna grow with them reasonably well,” he said. Unfortunately “there’s not a lot of understanding (about) what factors go into that.”
Another issue for doctors is the need to consider “the influence of immunosuppression on growth and development” when treating pediatric patients, Sweet said, referring to the anti-rejection medications organ recipients must take for the rest of their lives.
The “critical care management team did a great job supporting him until organs became available,” Sweet said. Spencer was put on a ventilator, and there was concern “that would tip him over an edge,” Sweet said.
Once he was admitted into the hospital on November 11, Spencer’s condition fluctuated for weeks. Tensions ran high in the hospital, and Kolman’s experience waiting for donor organs for his son had become “an emotional roller coaster.”
The reason? Spencer’s doctors – who knew that it could take 12 weeks to get a heart-lung donor – had begun to explore other medical interventions. This included transplanting only a set of lungs so Spencer “could have something to survive on and then roll the dice on his heart,” Kolman said.
Instead, he and Spencer made the decision “that we would wait as long as we could to get the heart and lungs that he needed to live … basically push the envelope as far as we could.”
“By a miracle of God – and miracle of organ donation – all of a sudden on November 29, I got a call from the transplant coordinator that they’d found a donation for Spencer,” Kolman said.
The history
The history of this special surgery begins with the heart, according to Dr. Thomas G. Peters, a professor emeritus in the department of surgery at the University of Florida College of Medicine.
“The first successful heart transplant was carried out in 1968 by Dr. Christiaan Barnard at a hospital in South Africa,” said Peters, who has published a book on the history of transplant surgery. Barnard’s patient, at Groote Schuur Hospital in Cape Town, survived for only a short period of time after surgery, coming off the ventilators for just 18 days until he succumbed to pneumonia.
“That heart transplant was the event that showed the world that it was more than technically feasible to transplant a heart,” Peters said.
In the 1960s, several successful lung transplants occurred, according to Peters. “I think the first successful lung transplant was done by Dr. James Hardy in 1964 at University of Mississippi. Dr. Hardy actually took a lung from the morgue – there wasn’t even any preservation – and he transplanted it into a prisoner.”
The patient lived 17 days before dying, not of a surgical complication but an entirely separate cause, according to Peters.
Meanwhile, though experimental kidney transplants had been performed in the early 1900s, the first successful kidney transplant was performed by Dr. Joseph Murray, who later won a Nobel Prize, in Boston in 1954, according to Peters. (An earlier version of this story incorrectly stated the date of this surgery.)
Dr. Norman Shumway performed the first heart-lung transplant in 1981, made possible in part by refinements in immunosupressive therapy, Peters explained.
“In the 1980s, a drug called cyclosporin emerged, and that drug changed the entire practice of immunosuppressive therapy because it could reliably prevent rejection in most cases,” said Peters.
Today, organ transplants are increasingly common. In 2016, there were 33,606 transplants, an 8.5% increase over 2015 and up 19.8% since 2012, according to the United Network for Organ Sharing in the US, which serves under federal contract and brings together medical professionals, transplant recipients and donor families across the country.
Though it is more rare, a total of 4,614 heart-lung transplants have occurred worldwide between 1985 and June 2015, and of these, 712 were pediatric surgeries, according to the International Society for Heart & Lung Transplantation, a nonprofit professional organization dedicated to improving the care of patients with advanced heart or lung disease.
Within the US, more than a thousand heart-lung transplants (1,199) have been performed since 1988, with a small fraction (199) of the total patients children like Spencer.
According to Eghtesady, Spencer’s operation was an “en bloc” transplant, in which the heart and lungs are not separated but transplanted together. In some cases, these surgeries can take up to 12 hours, though Spencer’s surgery took less than five hours.
St. Louis Children’s Hospital had taken a risk with Spencer, but “it turned out that was the correct assessment, and it went well,” Eghtesady said.
Time to keep up
“I think Spencer’s quality of life is going to improve substantially,” Eghtesady said. Based on data from past operations 80% to 90% of patients have substantial improvement in their ability to carry out routine daily activities, including walking and generally taking care of himself.
“He can now have a life,” Eghtesady said, adding,”the future really depends on how he does and how his body accepts or rejects the graft.” Most often, it’s the lungs part of the equation, not the heart, that causes complications after a transplant. Still, some patients have lived 20 years or so with a lung transplant, he explained.
According to Sweet, all organ transplants are a balancing act.
On the one hand, you must constrain the immune system so the organ isn’t rejected, and on the other hand, you must not suppress the immune system too much, or an infection will create significant difficulties.
For now, the team at St. Louis is monitoring Spencer for signs of infection and evaluating how well his lungs are functioning. “The hope is, you’ll beat the odds if you make it to five years, and you’ll be really lucky if you make it to 10 years,” Sweet said. “We like to think that children who survive 10 years are likely to continue to do well.”
Both he and Eghtesady say that the future is uncertain for Spencer, but the first year is critical and usually indicates whether a patient will do well.
“My hope and my prayer for him is that he’s among the 50% that does well for an extended period of time,” Eghtesady said.
“In the meantime, there’s a lot of research that’s still going on to try to figure out if there’s a way we can prevent chronic graft rejection so patients can live longer,” Eghtesady said. “My motto is, you just have to make the most of every single day.”
According to Kolman, Spencer’s progress has been “phenomenal.” Before the surgery, Spencer couldn’t walk up a flight of stairs, “even on oxygen, I would have to carry him up and down.”
“The other day ,he just walked a mile on the treadmill,” Kolman said. “I feel the curve coming where he’s going to like pass me up and I’m going to have to huff and puff and try and keep up with him.”
Meanwhile, Spencer is thrilled to no longer need equipment.
Follow CNN Health on Facebook and Twitter
“After the operation, when I was able to start walking around, it almost felt completely different because it was so much easier,” Spencer said. “I am amazed.”
Though his voice has been hoarse (due to the ventilator breathing tube), his throat does not feel sore, and he expects his voice will return soon. After the surgery, he had trouble with his gastrointestinal system, but now he’s been told his recovery and progress are going well.
“Better than they expected,” Spencer said.
For now, he’s going to the hospital a few days each week for tests. “I’m living at home in St. Louis until they say I can go back to Chicago. My dad and I hang out and watch sports together, movies. … I’m catching up on schoolwork.”
As his father sees it: “Spencer is not a fighter but a gladiator, thrown into this not by choice but by necessity for survival.”
Finally, the time has come for this gladiator to keep up.