(CNN)I am a pediatric nephrologist (kidney physician), specializing in transplant, in New York City, and even though it had been 15 years since I had taken care of adults, I jumped at the opportunity to join the front lines of the Covid-19 pandemic and volunteered for redeployment in late March.
It was my own way of saying thank you to the city that gave me my medical degree. But from the moment I sent the email requesting to volunteer, my sleepless nights began. When would I be called? Would I know what to do? Who would take care of our kids?
I was redeployed for one week, after which I returned to inpatient service in pediatric nephrology.
In that week, I realized that we can all be empowered to rise up, to trust ourselves and respond to those in need. This is why I became a doctor.
When I saw the text message from my chief on the morning of May 8 that said that I would be redeployed to the adult ICUs of our hospital, New York-Presbyterian/Columbia University Irving Medical Center, I felt my heart skip a beat.
Read More
I was physically ready to push past my comfort zone, but was I emotionally and mentally ready? That same morning, I called my close friend from college who happens to be an adult cardiologist. She told me to take a breath. She said, "Everyone is working toward a common goal. Even if we are out of our comfort zone, there is always someone to help."
Many years ago, we had taken the same pre-med and MCAT classes, entered and graduated different medical schools and somehow found ourselves years later practicing in the same city, in the same hospital system.
Little would we know in college that our lives would be intertwined in such a path during a crisis. She herself had been redeployed for weeks, far from her children to decrease exposure, and here I was, asking her to review EKG patterns in preparation for my "new life" on the following Monday.
I spent eight hours the weekend before studying medical management in coronavirus and squeezed into my head as much adult medicine I could muster. My husband, who is also a doctor, tried to teach me three years of his internal medicine residency in one crash course weekend before I left for my hotel, where I would self-isolate to minimize the risk of exposing my family to the coronavirus.
Then it hit me: I had never been past the doors of the cafeteria across the street at our adult hospital.
I was going to enter one of the main Covid-19 units at New York-Presbyterian (a system with one of the highest number of coronavirus inpatients in New York). I felt myself flushed, eager, a little nervous. I had mistaken the start time of the shift and found myself 30 minutes late -- which made me less confident in the endeavors of the day.
During this crisis, my pediatric nephrology colleagues and I had been adapting our skill sets to care for adult patients as our pediatric ICUs became transformed into adult coronavirus units at the peak. I saw all my pediatric colleagues rise up to the challenge, riding along the edge of the city's health care system's abilities as we also started seeing the virus affect children in new forms. Taking care of such adults through the lens of a nephrology consultant in my children's hospital was one thing, but returning to adult ICU care was going to be another task.
I had to re-learn how to be a resident, including pre-rounding (reviewing and organizing all the data and vitals from overnight) and preparing for presentations to the morning ICU team. When I looked around, I began to see familiar faces: pediatric trainees and my pediatric hospitalist colleague who also had been redeployed. I was thankful to be around this group of self-selected volunteers (residents from physical medicine and rehabilitation, psychiatry, orthopedic surgery, ENT, etc).
At the eye of this storm was an intricate camaraderie between physicians, trainees, and nurses. We were led by a critical-care physician who empowered each of us to step up to this challenge and share expertise from our fields together to address management plans.
Throughout the days and nights, I constantly shifted mentally between three medical eras of my life: as a medical student with the curiosity to learn; as a resident, with the ability to recognize a sick patient and place orders rapidly when needed; and finally, as a faculty member, utilizing my inner strength to trust the confidence of my decision making.
Under supervision, I pushed my comfort zones in doing bedside procedures I had not done in years (placing feeding tubes, drawing blood cultures and arterial blood gases, performing bedside ECHOs to diagnose tamponade, etc) since this is what needed to be done.
As physicians we are type-A perfectionists, even for something we have not done in years. I wanted these patients to get the same perfection I aim for with my kidney biopsies. They deserved no less.
As a pediatrician, I have grown accustomed to providing updates to fathers and mothers. During my redeployment, I realized I was less prepared to speak with spouses and partners. These patients were no longer my juniors -- but now peers in my same age group.
Each day we reached out to close family members to give updates. In this crisis, visitors were no longer allowed, so video imaging served as a connection for these families to see their loved ones. Sometimes family members would call their sick loved ones on Face Time and play music for them. The sound permeated through the ICU glass doors.
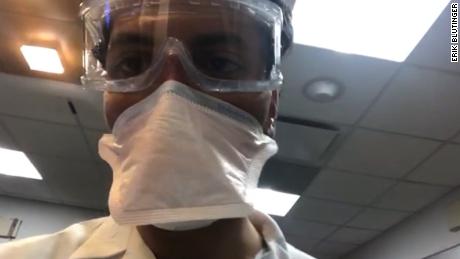
Each of these patients had a story, a family, and a life outside these doors. Our goal was to get them one step closer to home. Since these patients' human contact was relegated to hospital staff, I would try to try to provide an emotional bridge by sitting at their bedside, holding their hands and speaking to them while donned in my full isolation gear.
I hoped hearing words of encouragement would carry more weight as a fellow human -- not just as a physician. I could never replace a loved one at the bedside, but we all needed to continue this fight.
I still find myself reflecting on my adult patients from across the street, the memory of my experience still deep to my core.
Get our free weekly newsletter
Sign up for CNN Opinion's new newsletter.
Throughout my time there, as I watched partners worry about their significant others, I thought of my own husband who has had a deluge of sleepless days and nights as an infectious disease specialist in the last few weeks. Now, for our 10-year anniversary -- which happened during my redeployment -- we celebrated with a role reversal of our medical training: He taking care of the "pediatrics" side (our kids) and me in the MICU taking care of adult patients.
Each year when we celebrate our anniversary in the future, I will think about this experience and remember that I was exactly where I was supposed to be. I was in my city, in my hospital, in my zone doing what I love: practicing medicine in all its forms.